On September 26th CMS released a Medicare Advantage (MA) Plan Memo updating specifics surrounding HIPPS code sets related to PDPM implementation, launching today, October 1, 2019. (Memo 1) These details are inclusive of iSNP and MyCare.
The Memo relates to two previous CMS MA Plan Memos in 2014. (Memo 2) (Memo 3)
More specifically, the memo clarifies the required submission of HIPPS coding on each MA enrollee SNF claim:
- The continued usage of previously approved HIPPS coding,
- New HIPPS coding, derived from the PDPM,
- Encourages payer communication distribution to providers and
- Provides a CMS source for additional information if needed.
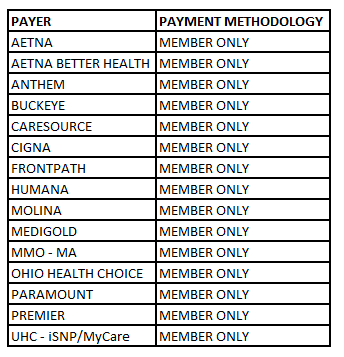
Access Advantage has been in communication with each contracted Managed Care Plan since August. Last week we provided to our Member’s an updated roster confirming the October 1st adoption of PDPM by all Plans with the exception of Premier and Medigold. (See below chart)
We anticipate additional communications by Payers over the next several days and weeks and will update all Member’s as it becomes available. We will also update our chart accordingly, such that it will be useful as a staff reference.
Please let us know if you have any questions. Our Service Box at service@accesselite.com is routinely monitored throughout the day or you may contact Rachel Pfahler, Director of Network Development and Engagement at rachelp@accesselite.com for assistance.